IntroductionPalliative care is a practice discipline, which involves progressive and life-limiting illnesses such brain metastasis , chronic obstructive pulmonary disease, motor neuron disease [MND], and multiple sclerosis, each of which can benefit from the involvement of physiotherapy. Providing pain relief and management of distressing and debilitating symptoms, palliative care improves the quality of life (QoL) for patients with a life-limiting illness and their families. Helping integrate the psychological, social, and spiritual aspects of holistic care, palliative care manages patients’ symptoms and pain levels, providing relief from distress and ultimately, facilitating improved function.
All patients regardless of their diagnosis should be able to access palliative care appropriate to their current individual needs, to allow this to happen an integrated approach to palliative care is required.The rise in the number of elderly people, especially those who have little home support, makes palliative care even more vital. People dying from stroke, dementia, or multi-system failure need to be guaranteed the same level of care as those that have a diagnosis of cancer.
Palliative care was initially seen as ‘terminal care’. Its scope has recently broadened and the concept of ‘rehabilitation’ in palliative care is becoming more widespread. Pain relief and the control of symptoms are employed where rehabilitation is not appropriate, depending on the stage of the illness.
Physiotherapy in Palliative Care: The Need for Learning and Development in This Area
Allied health and rehabilitation in palliative care are well established. Meeting patients’ physical, psychological, social, and spiritual needs, palliative care rehabilitation fits the adopted bio-psycho-social approach to health care, suggested by the World Health Organization. Involving symptom management and treatment effect minimization in patients with progressive and irreversible illness, this essential service within health care must be utilized where appropriate, improving and maintaining patients’ and their families’ QoL. Physiotherapy aims to maximize movement and function when threatened by aging, injury, or disease, essential for optimal wellbeing.
Existing evidence, though in its preliminary stages, advocates the role of physiotherapists and rehabilitation in palliative care. Early referral to palliative care rehabilitation has been linked to higher-functioning patients, therefore appropriate referral to palliative care physiotherapy is critical for optimal and patient-centered care.
Despite the potential benefits of palliative care physiotherapy, evidence suggests a lack of palliative care patients receiving physiotherapy treatment. As a result, to the detriment of patients and the NHS (National Health Service UK), specialist palliative care teams may be failing to deliver patient-centered care, by failing to refer. Research suggests the reluctance of referral, by other allied health professions, due to the misconceived perception of the inappropriateness of terminally ill patients to rehabilitation.
In addressing this commonly altered perception of palliative care physiotherapy on a preliminary level, this self-study CPD (continuing professional development) package will demonstrate the vast capability and variability of rehabilitation in such a setting. With palliation, physiotherapy treatment aims to maintain QoL while alleviating stress from symptoms, in particular, pain, and effects from treatment. Palliative care physiotherapy has been found to positively influence QoL and perceived wellbeing in a range of palliative care populations, including cancer, HIV, neurological disorders, cardiopulmonary conditions, and mental illness. Palliative care physiotherapy specialists demonstrate extensive knowledge and vast experience working with life-limiting illnesses, with competency in responding to rapidly changing situations. A recent survey suggests training in end-of-life care settings was inconsistent across current UK undergraduate courses in medicine, adult nursing, occupational therapy, social work, including physiotherapy. Further research is needed to identify how to remove the barriers and improve the consistency of current training.
In response to staggering research on palliative care rehabilitation perceptions and lacking numbers of referrals, this self-study package has been designed as an educational resource for all allied health professionals in the United Kingdom (UK). The package aims to void a trough in knowledge, and degree of uncertainty or misconception, surrounding the referral of appropriate palliative care patients, to physiotherapy.
It is not exclusive to any one palliative care specialty area but can be adapted for a range of palliative care areas. While providing up-to-date factual information for allied health professionals, this package will endeavor to extend beyond the tangible requirements for referral to physiotherapy in palliative care. It will provide a sound explanation of necessary personal values and the importance of suitable communication skills, for interaction with patients and families in or being referred to palliative care.
Palliative Care SettingsEveryone facing a life-limiting illness will need some degree of supportive care in addition to treatment for their condition. Patients can receive palliative care physiotherapy at any time and at any stage of illness, whether it is terminal or not. It can be offered:
- In a hospice
- In the patient's home
- As a day patient in a hospice
- In a hospital
- In the community
Patient Needs and Our Role as a PhysiotherapistThe physiotherapist must consider the patient’s needs and wishes, along with their physical needs . Each individual will have different needs depending on how well they are handling their life-limiting illness. Robinson claimed that patients’ needs and priorities must be addressed for treatment to be successful. Patients may need education on how to cope and handle the situation as best they can to lessen the fear and anxiety, they have surrounding their condition. Worry and anxiety are two common psychological aspects associated with life-limiting illnesses. The entire MDT, including the physiotherapist, may be involved in the control of some of these symptoms, through education, maybe even just empathy towards the patient. Often when diagnosed with such illnesses patients can suffer from depression. This can regularly result in the individual becoming bedbound and inactive.
The needs of a patient in palliative care often include:
- To remain as independent as possible/maximize independence and daily function.
- To optimize and maintain quality of life (QoL) – determined by physical functioning and psychological symptoms.
- Reduction/control of the consequences of the illness .
- Coping mechanisms and self-management – to be in more control of their lives.
- To avoid secondary complications associated with life-limiting illnesses.
- Psychological support.
Communication Effective communication is paramount for interaction with patients and families in or being referred to palliative care. Palliative care physiotherapy specialists demonstrate extensive knowledge and vast communication experience working with life-limiting illnesses, with competency in responding to rapidly changing situations.
Appropriate communication follows the bio-psychosocial model and is a core priority for palliative care services concerned with the psychological and emotional well-being of the patient; including issues of self-esteem, insight into and adaptation to the illness and its consequences, communication, social functioning and relationships.
In a study by McIlfatrick, the needs identified by patients and their caregivers in palliative care included social support and the provision of practical care, respite care, psychological support, and information and choice. Therefore, knowledge of the patient’s diagnosis and any associated past treatments or conditions, to be able to plan the best physiotherapy treatment.
Common symptoms and Physiotherapy ManagementIn patients with life-limiting illnesses, symptom control and maintenance of function become crucial aspects of treatment. Palliative care aims to improve the QoL in patients faced with life-limiting illnesses. There is a role to be played in pain management and the ref of other distressing symptoms.
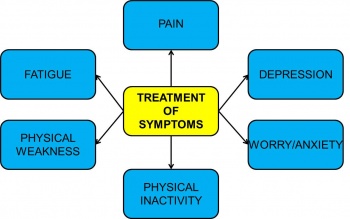
Pic: Common symptoms experienced by palliative care patients and physiotherapy treatment of these symptoms.
Physiotherapists primarily address the physical components of rehabilitation. With life-limiting illnesses, cancer, for example, there is also a psychological aspect, which we as physiotherapists may need to also address. The whole needs of the individual must be addressed.There are many forms of treatment that physiotherapists can employ in the management of patients in palliative care. The decision as to what option best suits each patient is quite personal and depends on the stage of the disease process and goals set. Goals are largely dependent on the stage the patient is at. Life prolongation can be a goal in the early stage of illness but as the illness progresses the goal can shift to optimizing QoL as opposed to prolonging it. Different treatments are suitable for the various phases of illnesses. These different forms of treatment provided by physiotherapists and their suitable phases are displayed in Table.
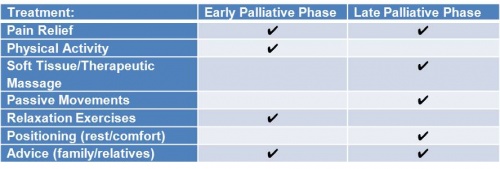
Table : Physiotherapy treatment and suitable phase during palliation.
- Pain relief – TENS, heat, massage, lymphedema treatment, and acupuncture are common forms of pain relief. Pain relief is often employed where rehabilitation is not appropriate.
- Passive movements – These are often used, in-bound patients.
- Physical exercise – This may positively affect depression and is currently emerging as a major aspect of the treatment of patients in palliative care.
- Soft tissue massage and/or therapeutic massage are used to relieve muscle tension and can often aid in easing the symptoms of anxiety.
Author: Sushanta Kumar Ghosh, Physiotherapy Specialist, DIU Medical Center


